It’s not only a ‘fatty’ liver but signals danger to other organs too
Hepatologist Prof. Madunil A. Niriella turns focus on newly-named MASLD
By Kumudini Hettiarachchi
Located beneath the rib cage in the right upper abdomen, it is the largest solid organ in the body. Vital for removing toxins from the blood supply, the liver maintains healthy blood sugar levels, regulates blood clotting and performs hundreds of other functions.

Prof. Madunil A. Niriella
A fatty liver – a build-up of fat in the liver cells – may not be just a liver issue but could be a danger signal of obesity, diabetes, hypertension and elevated abnormal cholesterol (atherogenic dyslipidemia – AD).
As all these are closely associated with metabolic dysfunction, Non-Alcoholic Fatty Liver Disease (NAFLD) has had a name-change to Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) to reflect the wide-ranging impact on the human body.
Explaining the name-change, the Senior Hepatologist of the Colombo North Centre for Liver Disease (CNCLD), Faculty of Medicine, University of Kelaniya, Prof. Madunil A. Niriella said that earlier in the diagnosis of NAFLD, there were strict restrictive criteria under which any other liver disease was excluded.
“It is the same disease but with a clearer definition and less-stigmatizing terminology. Now the MASLD definition is simpler and clearer – requiring only a demonstration of fatty liver plus 1 of 5 metabolic criteria. These metabolic criteria are overweight/obesity; diabetes; hypertension; and two types of abnormal blood lipids,” says Prof. Niriella who is also Professor in Gastroenterology, Department of Medicine, Faculty of Medicine, University of Kelaniya and President of the Sri Lanka Society of Gastroenterology.
Fatty liver is the “commonest” chronic liver disease in the world, with a prevalence of 32% among adults and an “alarming” prevalence of 60% (double the usual) among those suffering from diabetes, he says, as globally International NASH (Non-Alcohol Steatohepatitis) Day was commemorated yesterday (June 8). NASH is the more aggressive form of NAFLD.
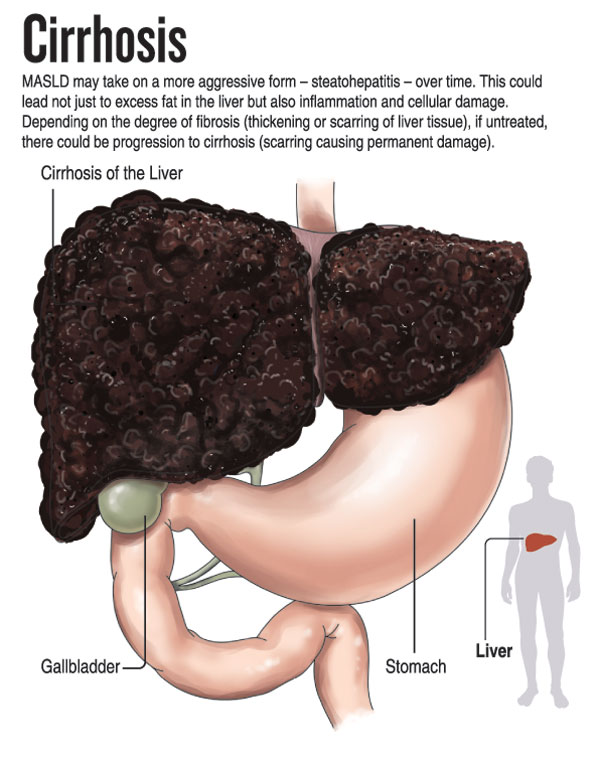
Pointing out that NAFLD turned MASLD is a spectrum of diseases, he explains that it starts asymptomatically in early childhood and adulthood taking on a more aggressive form – steatohepatitis – over time. The aggressive form is not just excess fat in the liver but also inflammation and cellular damage of this organ. Depending on the degree of fibrosis (thickening or scarring of liver tissue), if untreated, there could be progression to cirrhosis (scarring causing permanent damage) and the development of liver cancer.
How can one develop Steatotic Liver Disease, asks Prof. Niriella, giving the vulnerabilities as:
- A genetic predisposition (an increased chance of developing a disease based on genetic make-up), coupled with an unhealthy lifestyle
He goes onto reiterate that not everyone who is genetically predisposed would be hit by this disease as an unhealthy lifestyle, which can easily be changed, also plays a major role.
An unhealthy lifestyles means:
- Being physically inactive – lack of exercise and a very sedentary life
- A high-calorie diet of refined sugar – sugar-sweetened drinks and milk products
- A high-fat diet – processed foods such as sausages and bacon
“All these lead to weight gain and, in turn, to fatty liver,” he cautions, warning that if untreated for 20-25 years, the powerful liver may go into cirrhosis. However, this does not happen in all patients with fatty liver. There is an ‘at-risk’ group and it is very important to identify them.
Prof. Niriella describes how fatty liver is usually diagnosed “by chance” during routine ultrasound scanning for an abdominal ailment (including a urinary tract infection). Or it could be a routine blood test which may include the liver enzymes AST (aspartate aminotransferase) and ALT (alanine transaminase).
“If these scans and enzyme levels indicate a problem, we suspect Steatotic Liver Disease and there is a further evaluation – the ‘FIB-4’ (Fibrosis-4 or Index for Liver Fibrosis). This evaluation is made using the age of the patient as well as the AST and ALT and the platelet count,” he says.
- If FIB-4 is low – the patient can be reassured that there is no liver fibrosis and with proper lifestyle changes, the condition can be reversed
- If FIB-4 is high – an additional test would be required to find out the extent of liver fibrosis. This is a specialized ultrasound, the Transient Elastography (FibroScan), which has to be performed at a specialist centre
Explaining that of all patients with NAFLD, about 20-25% would have NASH and these NASH patients, if untreated, are at risk of fibrosis, Prof. Niriella says that all those with fatty liver would be advised on lifestyle modifications.
He holds out hope with weight loss – the weight loss targets would be 5% for those who have normal weight and 10% for those who are overweight and obese, to reverse liver damage in most patients.
The simple answer will be:
- A hypo-caloric diet which means 500 calories less than the daily requirements of that particular individual, while excluding sugars and limiting fatty food
- At least 150 minutes of moderate to intense exercise – 30 minutes a day for five days every week of brisk walking, jogging, cycling or swimming with twice weekly muscle strengthening
- All those with fatty liver should avoid alcohol as it would accelerate liver fibrosis
- Have adequate sleep of 6-7 hours each night
- As research has indicated, 2-3 cups of unsweetened black coffee daily are helpful. There is no research on tea and liver disease yet
With Fatty Liver Disease closely linked to being overweight [having a Body-Mass Index (BMI) between 23 and 25] or obese (having a BMI of over 25), the same risk factors aid the development of Cardiovascular Diseases (CVDs – heart attacks and stroke). As such, the treatment of fatty liver helps cut the risks of CVDs, it is learnt.
Prof. Niriella says that as the basic treatment and management of fatty liver of those not at-risk is weight loss, these patients can be managed by their General Practitioners (GPs). However, those at-risk with a strong family history of non-alcoholic cirrhosis and non-alcoholic liver cancer and multiple CVDs, identified with a high FIB-4 evaluation should be under the care of a specialist.
Referring to medications for those at-risk, he says that up to this year there was no regulatory approved drug for MASLD. This year, though, in America, the US Food and Drug Administration (FDA) has approved the first drug treatment.
But it may take a long time to be available in Sri Lanka, taking into consideration the high cost factor and that it is not registered here, he adds.
How to tackle fatty liverProf. Madunil Niriella’s message is:
- Everyone with fatty liver may not develop cirrhosis. However, as it is a multi-system disease, the person may be at risk for Cardiovascular Diseases (CVDs) such as heart attacks and stroke.
- This is why those with fatty liver need multidisciplinary management with the input of a hepatologist, an endocrinologist, a physician to manage CVDs, a nutritionist for diet and a lifestyle coach for exercise.
Quoting a study conducted over 15 years ago in Sri Lanka on fatty liver prevalence, Prof. Niriella says:
- 33% in the urban population had fatty liver
- 10% in the rural population had fatty liver
These data may have changed most likely to higher numbers, he adds.
The Dietary Therapy being put forward is:
- Restricting energy with a hypo-caloric diet
- Encouraging a Mediterranean diet pattern – fresh fruit and vegetables, whole grain or cereal rich in fibre, nuts/seeds/legumes, fish or white meat and olive oil
- Minimizing the consumption of saturated fatty acids including ultra-processed food and red and processed meat and also sweets, high fat/sugared dairy products and sugar-sweetened beverages
- Limiting alcohol and avoiding smoking
